
When Beth Kaczmarek and her husband Bryan Craig moved back to her hometown of Santa Fe, New Mexico. Beth planned on delivering their baby in the same hospital where she was born. Their daughter Eloise, however, had other plans.
“We were living in Napa County, California when we decided to start a family,” said Beth, 38. “We had moved back to the States after living abroad and I was in the midst of a big editorial project.”
As a writer and wine educator, Beth was consulting with the 3rd edition of The Wine Bible. Her husband Bryan, 39, continued his work as a CPA with a private accounting firm providing auditing services for government contracts.
“Once we knew we were having a baby, we decided to move to Santa Fe where my family has lived for 45 years,” she said.
As her first pregnancy progressed into the third trimester, Beth had not experienced any problems.
“Everything seemed normal,” she said. “Despite my advanced maternal age, as they like to label those of us over 35 years old, I had few complications. We were very excited and happy; everything seemed to be going so well.”
A conversation with one of her doctors did hint at a possible difficulty.
“I had COVID four months into my pregnancy,” said Beth, “and one of the doctors mentioned a recent study that some pregnant women who contracted the coronavirus had problems with placental abruption – when the placenta separates from the inner wall of the uterus before birth.”
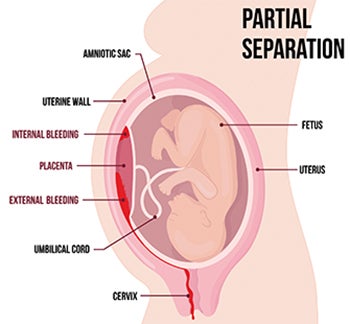 Placental abruption can deprive the baby of oxygen and nutrients and cause heavy bleeding for the mother. The study, which doesn’t yet have enough data for a conclusive result, stated that COVID-19 may cause the placenta to age quicker than the child. Without the coronavirus, the national rate for placenta abruption in all pregnancies is only 1%.
Placental abruption can deprive the baby of oxygen and nutrients and cause heavy bleeding for the mother. The study, which doesn’t yet have enough data for a conclusive result, stated that COVID-19 may cause the placenta to age quicker than the child. Without the coronavirus, the national rate for placenta abruption in all pregnancies is only 1%.
Beth’s doctors said they would monitor her condition closely and would schedule a few more ultrasounds along the way to make sure the placenta remained safe.
“We’ve got to go!”
In case complications arose, Beth and her doctors had a plan in place for how and where the baby would be born.
If Beth started going into labor and the baby was less than 32 weeks along, Beth would travel to Lovelace Women’s Hospital, since the Santa Fe hospital could not care for babies under 32 weeks. If that happened, Beth knew that she would give birth by Caesarean section surgery in Albuquerque.
During the 30th week of her pregnancy, there was a rare, dark and stormy night in Santa Fe when Beth knew the baby was on the way.
“I started contractions around midnight and knew by 4 a.m. that it was time to go to the hospital,” Beth recalled. “With the possibility of placenta abruption, in order to insure the highest chance of survival of our baby and me, we needed to go right away. That’s when they put me in an ambulance for the one-hour drive down Interstate 25 to Albuquerque.”
Beth was given medication that would help slow the contractions. With the possibility that her baby would be born soon, she was also given shots to help her baby’s lungs develop.
When Beth arrived at Lovelace Women’s Hospital later that morning, she was admitted to a room and given medication to slow down the contractions. The plan was to keep her in the hospital and see if the baby could gestate inside of Beth for another 3-7 weeks.
“The staff at Lovelace was great. They did everything they could to keep me comfortable and slow down contractions. I was hopeful it would work, but later that night the contractions started again,” she said.
Her doctors continued to monitor the heart rates of both Beth and the baby, but soon it became apparent that the C-section surgery would be needed soon, as they had done everything they could.
“Dr. Regan Riley, the surgeon, came in and saw that with the new contractions, the baby’s heart rate was dropping, which decreased the amount of oxygen flowing to the baby,” Beth explained. “She said they could try to deliver the baby naturally, but the baby might not survive. Dr. Riley said, ‘We can do a C-section in 20 minutes, but we’ve got to go now,’ so I said ‘Let’s do it!’”
The Cesarean surgery was completed successfully without any complications around 5 a.m. Beth and Bryan had not asked to know the gender of their baby beforehand, so they were thrilled to hold their 30-week-old, 3-pound, 9-ounce baby girl Eloise that morning.
Weeks in the NICU
Since Eloise was born prematurely, the staff immediately placed her in a heated isolette in the Neonatal Intensive Care Unit (NICU) at Lovelace Women’s Hospital.
 She was connected to a CPAP (Continuous Positive Airway Pressure) machine to help her underdeveloped lungs to breathe. The doctors also inserted a feeding tube directly into her stomach for nutrition until she was able to suck and take breast milk.
She was connected to a CPAP (Continuous Positive Airway Pressure) machine to help her underdeveloped lungs to breathe. The doctors also inserted a feeding tube directly into her stomach for nutrition until she was able to suck and take breast milk.
These steps were very important for her development because, during the surgery, Dr. Riley found evidence that the placenta was starting to separate from the uterine wall.
Through every step in their journey, Bryan was right there with Beth and their new baby girl.
“Lovelace Women’s Hospital is very accommodating to spouses,” Beth said. “Most of the rooms in the maternity ward has either a pullout sofa or a big chaise lounge that turns into a single bed. There was always room for Bryan wherever I was, so it was really nice to have a private room with your partner there to deal with all the stress together.”
During the first two intensive weeks in the NICU, Eloise was under the care of nurses who only had two children to care for each shift.
“I remember feeling so cared for by the nurses,” said Beth. “Eloise was hooked up to all these tubes and machines and there were so many beeps and buzzes that I didn’t understand. But all the nurses, including Kim and Sarah B, have such nurturing spirits. We didn’t feel like visitors to the NICU, we were really part of Eloise’s care team.”
Another nurse, Lydia Walker, served as a lactation consultant and met with Beth within 24 hours of delivery. “She made a huge difference in getting my milk supply coming, even at 30 weeks. She got all the supplies for me, but it was her positive attitude that made it all much easier.”
Beth also had high praise for the skill of her surgeon Dr. Regan Riley and for Dr. Zuzana Novak, head of the NICU. “Dr. Novak was so approachable and so comforting,” Beth said. “I felt like I could ask a question to any doctor or nurse and they gave me the time and the answers. This emotional support, in addition to the medical care, really made our stay at the hospital special. You don’t find that at every hospital.”
Beth recovered from her surgery and remained in the hospital for five days. “It was supposed to be four days,” said Beth, “but I started having higher blood pressure readings. The doctors were concerned about preeclampsia, which could also have been a factor in Eloise’s premature birth. So I stayed a fifth day to give the blood pressure medication time to work. I was just happy to stay and have another day close to Eloise!”
As for Eloise, Beth and Bryan expected her to remain in the hospital until her expected due date – a total of 10 weeks. However, Eloise began to thrive under the care of the NICU nursing staff.
“Eloise started breathing more on her own, so they replaced the CPAP machine with a simpler oxygen tube around her nose,” said Beth. “When we saw that she was getting stronger and that she just needed to put on weight, they took the feeding tubes out. That’s when we taught her how to feed on her own by taking a bottle or the breast. She did really well with that.”
Home at last
Eloise progressed to a healthy weight and was released from the NICU at 36 weeks. Now home in Santa Fe, she still sees a couple of specialists to monitor her development.
“We have her regular pediatrician appointments,” said Beth, “but there are also visits from an occupational therapist to monitor her abilities to sit up, grab things, etc. and a nutritionist to monitor her diet, eating habits, etc. She keeps meeting milestones and is already sitting up relatively well with support.”
Every now and then, photos from when she was born will pop up and remind Beth and Bryan how much Eloise has developed.
“I saw some photos from that time and it was almost shocking to look back at where she was,” Beth said. “She was so tiny, so frail, so vulnerable, and now she's healthy, fleshy and laughing. She's just a wonderful baby.”
To read how Lovelace Women’s Hospital can care for you and your baby, visit our website or call us at (505) 727-7677.




