Everything was going as planned.
A few weeks into the third trimester, Elizabeth and Jose Villar went to her regular obstetrician appointment, hoping to hear more about when their twins would be born.
“You should expect to go full-term with your babies,” said the obstetrician, “but we may induce you a week or two earlier to guard against any complications since this is your first pregnancy.”
Relieved, the two 35-year-old Albuquerque residents relayed the plan to their families who lived a few hours away. Jose also planned to update the staff at the University of New Mexico where he is the director of college enrichment and outreach programs.
“So going into the weekend, we thought we had about nine more weeks left,” said Elizabeth.
Serious complications
Over the weekend, Elizabeth wasn’t feeling well. She only stood to shower and get dressed, but mostly stayed off her feet with her legs elevated. These self-care remedies worked well on Saturday and Sunday, but by Monday evening she could not find any relief from pain in her ribcage.
“We went to the Emergency Department at Lovelace Women’s Hospital because things didn’t feel right,” explained Jose. “As it turned out, it was a good thing that we were there.”
“When we got to the hospital,” recalled Elizabeth, “the staff checked my blood pressure and it was going through the roof! They also took some blood and urine to send to the lab for testing.”
The staff closely monitored Elizabeth’s blood pressure and the number of red blood cells, liver enzymes and platelets.
“They were testing her blood every 30 minutes, or so,” Jose explained. “They would send the sample to the lab and we would wait 15 to 20 minutes for the results. After the first blood draw, the doctors said it looks like the babies will come early, around 34 weeks. After each lab test, the numbers got worse. They thought we would deliver in a month, then two weeks, then a week, and then they decided that an emergency cesarean section had to be performed as soon as possible!”
The staff quickly prepped Elizabeth for surgery while Jose was shown to a waiting room.
HELLP Syndrome
Elizabeth’s blood tests showed the doctors that she had HELLP Syndrome. A type of preeclampsia, HELLP syndrome is a very rare pregnancy complication that occurs in fewer than 1% of all pregnancies.
The name HELLP Syndrome stands for the following complications that affect the mother’s health:
- H: Hemolysis – the breaking down of red blood cells which carry oxygen from your lungs to the rest of your body
- EL: Elevated liver enzymes – chemicals that speed up body reactions, such as breaking down proteins
- LP: Low platelet count – the components of your blood that help with clotting
Once the diagnosis was made and the decision for immediate surgery was announced, the doctors had little time to spare. Elizabeth was put under general anesthesia for the surgery, but her care team had to act quickly to get the babies out before they felt the effects of the anesthesia. In addition, they had to minimize blood loss from Elizabeth, as HELLP Syndrome could cause her organs to shut down without adequate oxygen-rich blood.
“The nurses told me afterward that the babies were born a minute apart,” said Elizabeth. “As soon as I fell asleep, the doctors had two, 60-second intervals to get the babies out. Everything happened so quickly. We got to the hospital at 2:30 in the morning and they were out at 5:30 a.m.”
Meanwhile, Jose was in the waiting room, wondering what was going on in the surgery room.
“I was so concerned for her and the twins,” he said. “This was our first pregnancy and it wasn’t going as expected. As I sat there, time was passing and I was getting a little worried. Finally, the doctors came out and I could tell that they were somewhat excited and tired after performing the surgery. They appeared to relax a bit, so I did too.”
Another emergency
Suddenly an alert came over the intercom, informing the doctors to return to the operating room.
“The doctors were frantically putting on fresh scrubs and running back through the doors. I was freaking out and didn’t know what was happening, so I asked one of the nurses to please go inside to see what was going on. When she returned, I said, ‘Please tell me what is really happening.’”
The nurse answered, “They thought everything had gone well, but Elizabeth is still bleeding a lot.”
A hemorrhage – heavy bleeding – is one of the serious complications of HELLP. Fortunately, the doctors were able to insert a balloon into Elizabeth’s uterus. The balloon pressed up against the uterine wall, compressed the lining and helped blood clots to form and stop the bleeding.
High praise for the doctors and nurses
Through it all, Elizabeth and Jose were very grateful for the care they received during the early morning hours. “The doctors and nurses were amazing,” said Jose. “Overall, we trusted the professionals, but it was a very scary event.”
“There was one nurse, I think her name was Tinder,” said Elizabeth. “She could hear our conversations and how scared we were, so she just came up to us and said, ‘Can I pray with you? Are you okay with that?’ And we said, ‘Absolutely.’ It was so awesome to have her there with us during that time.”
After the surgery, the nurses brought their son out in an incubator and wheeled him up to the Neonatal Intensive Care Unit (NICU). Right after that, their daughter came out and went upstairs too.
“There were some high peaks of emotion during that time,” recalled Jose. “I so full of excitement when I saw our twins during well, but then it all changed to despair when Elizabeth was bleeding. I was trying to balance all of these emotions, but there was really nothing I could have done except pray.”
Home for Christmas
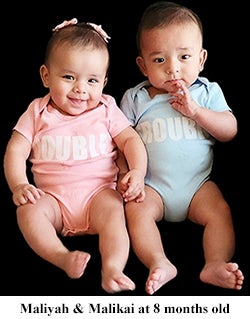
“We had celebrated Thanksgiving in the NICU, but for Christmas, we really wanted to be home together as a family,” said Jose. “We were concerned that Malikai would have to remain behind, but we were able to bring him home at the same time with oxygen to help him breathe better.”
Today the twins are thriving, hitting their growth milestones and catching up to their appropriate height and weight. The parents are even noticing their interesting personalities.
“They are doing great,” said Elizabeth. “Both are eating and sleeping well. You can’t even tell they were preemies. As for their personalities, Malikai is a little goofball! He is always laughing and likes to be the center of attention. Maliyah, on the other hand, is more reserved and a little shy, but she is also the sweetest little girl you’ve ever met. She doesn’t stop smiling!”
For more information about our birthing services, especially our neonatal intensive care unit, visit our website or call us at 505.727.7677.